Hierarchical Condition Categories (HCCs) are groups of diagnoses within disease categories that impact a patient’s risk adjustment factor (RAF) and reimbursement. HCCs help monitor the overall health status and predict the cost of care a patient is likely to receive based on the active conditions of that patient. The Risk Adjustment Payment Model is a prospective payment system, meaning that payments are based on HCCs reported in a previous year.
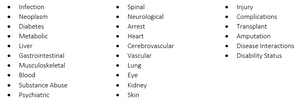
Not all diagnoses carry a risk adjustment value. Out of 71,932 ICD-10 diagnoses, only 10,860 are assigned to an HCC. HCCs are conditions that require ongoing care and management and are identified in coding manuals with an HCC icon. These typically include chronic conditions and permanent status conditions like transplants and amputations. The 2016/2017 Hierarchical Categories include:
Within each of these categories, diagnoses are weighted with higher scores prevailing over or “trumping” diagnoses with lower scores. Since only the highest score is reported in each hierarchy, it is crucial to code diagnoses to the highest level of specificity and accuracy to ensure reimbursements reflect the patient’s actual health status. For example, a stage 2 pressure ulcer has a higher score and trumps an unspecified pressure ulcer. If documentation did not specify the stage or a coder simply didn’t select the correct code, this patient’s total RAF score would be inaccurate and result in a lower reimbursement.
Understanding the importance of HCCs and how they contribute to reimbursements is great motivation to begin and/or continue Clinical Documentation Improvement efforts. For a crash course on HCC Coding, contact us today to learn about LHA’s HCC Boot Camp.
Content retrieved from: https://lighthousehealthcareadvisors.com/post/the-basics-of-hccs.